Intestinal Permeability
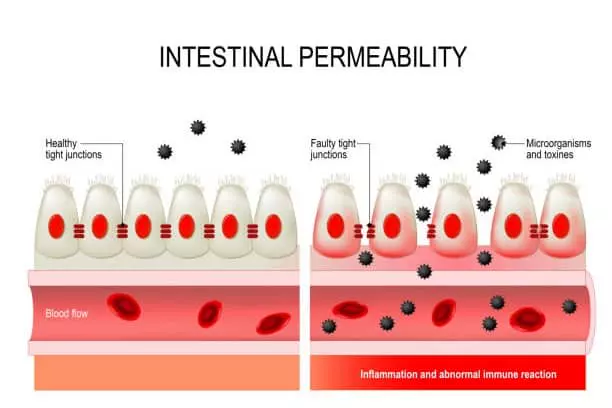
A condition known as intestinal permeability occurs when the junctions in the gut epithelial wall become porous, enabling material from the lumen to translocate into the bloodstream, other organs, or adipose tissue.
Everyone has semi-permeable intestines. Our intestines’ mucous lining is made to allow water and nutrients from food to be absorbed into the bloodstream. However, some persons have hyper- or incleased intestinal permeability. That means their guts let more than water and nutrients through — they “leak”.
Certain chronic gastrointestinal diseases have been linked to leaky gut syndrome, which allows bigger, possibly harmful molecules to pass through. Your intestinal lining’s role in serving as a barrier to bacteria and other infectious organisms inside the gut is one of its primary functions. This barrier is an important agent in your immune system.
Intestinal Permeability and Inflammation
Increased intestinal permeability, sometimes known as “leaky gut,” is linked to a wide range of diseases, including inflammatory bowel disease, dermatitis, autoimmune diseases, food sensitivities, autism, learning disabilities, and many more.
Because the intestines’ damaged barrier allows poisonous substances to enter the bloodstream and poison the body, this “leaky gut” leads to diseases. If a person additionally has intestinal overgrowth of bacteria or a high concentration of certain bacteria that create toxins, this will be exacerbated!
The gastrointestinal tract has two main functions:
- to digest and absorb important nutrients for the body’s growth and function, and
- to act as a barrier to keep harmful substances, immune compounds and microorganisms (bacteria, parasites etc.) from entering the blood.
When the integrity of this intricate system is impaired and there is greater intestinal permeability, illness can quickly arise. Increased intestinal permeability, commonly referred to as “leaky gut,” is linked to a number of diseases and ailments, including autoimmune disorders, autism, food sensitivities, inflammatory bowel disease, and jaundice.
Intestinal Permeability Assessment
Intestinal Permeability Assessment is an effective noninvasive gastrointestinal test assessment of small intestinal absorption and barrier function in the bowel.
The small intestine performs the dual roles of being an organ of nutritional absorption and digestion as well as a strong mechanical and immunological barrier against the overabsorption of bacteria, food antigens, and other macromolecules.
Chronic gastrointestinal imbalances as well as numerous systemic diseases are linked to both malabsorption and increased intestinal permeability (also known as “leaky gut”).
Leaky gut, or increased intestinal permeability, in the small intestine can:
- Increase the number of foreign compounds entering the bloodstream
- Allow bacterial antigens capable of cross-reacting with host tissue to enter the bloodstream, leading to auto-immune processes
- Enhance the uptake of toxic compounds that can overwhelm the hepatic detoxification system and lead to an overly sensitized immune system
There has been evidence of leaky gut in a wide range of diseases, including:
- Inflammatory Bowel Disease (IBD)
- Food allergy
- Inflammatory joint disease
- Chronic dermatologic conditions
According to research, the increased intestinal permeability seen in people with vasculitis, rheumatoid arthritis, and ankylosing spondylitis may play a significant role in the pathogenesis of these diseases.
On the other hand, decreased permeability seems to be the main reason for malabsorption, which leads to malnutrition and failure to thrive. Due to damage to the microvilli, permeability to big molecules may rise in some small intestinal disease states, such as gluten-sensitive enteropathy, whereas permeability to tiny molecules may fall.
As a result, nutrients are even less readily available to help the body detoxify the antigens that are constantly flooding it.
Intestinal Permeability Causes
Intestinal permeability occurs when the gut lining becomes overly porous. Factors that contribute include:
- Dietary Factors
- High intake of processed foods, sugar, alcohol, and gluten.
- Low-fiber diets that disrupt gut microbiota balance.
- Medications
- Overuse of NSAIDs (e.g., ibuprofen), antibiotics, and antacids.
- Gut Infections
- Conditions like small intestinal bacterial overgrowth (SIBO), H. pylori, or yeast overgrowth.
- Stress
- Chronic psychological or physical stress weakens the gut lining.
- Toxins
- Exposure to pesticides, heavy metals, or pollutants.
- Chronic Inflammation
- Diseases like Crohn’s disease or celiac disease.
- Autoimmune Disorders
- Conditions like lupus, multiple sclerosis, or type 1 diabetes may exacerbate leaky gut.
Intestinal Permeability Symptoms
Symptoms may vary widely and include:
- Digestive issues: bloating, diarrhea, or constipation.
- Fatigue and low energy.
- Brain fog or difficulty concentrating.
- Skin conditions: acne, eczema, or psoriasis.
- Joint pain and inflammation.
- Food sensitivities or intolerances.
- Mood disorders: anxiety or depression.
- Autoimmune flare-ups.
Increased Intestinal Permeability Meaning
Increased intestinal permeability indicates that the gut barrier, normally selective about what it absorbs, has become compromised. This allows harmful substances (toxins, bacteria, and undigested food particles) to enter the bloodstream, potentially triggering systemic inflammation and immune responses.
Intestinal Permeability Test
How to Test for Intestinal Permeability:
1. Clinical Tests
- Zonulin Levels: Zonulin regulates gut tight junctions. Elevated levels suggest permeability.
- Lactulose/Mannitol Test: A urine test to measure the absorption of these sugars, which indicates gut integrity.
- Stool Analysis: Evaluates gut microbiome health, inflammation, and infection markers.
- Blood Tests: Assess inflammation markers (e.g., CRP) or immune reactions to food proteins.
2. At-Home Tests
- Some labs offer mail-in tests, such as:
- Zonulin stool tests.
- Food sensitivity panels to identify inflammatory triggers.
- Stool or urine tests for gut health.
- You can also self-assess symptoms and track dietary or lifestyle changes to evaluate improvement.
Intestinal Permeability Treatment
Treatment for Intestinal Permeability:
- Dietary Interventions
- Elimination Diets: Remove common triggers like gluten, dairy, and sugar.
- Anti-inflammatory Foods: Incorporate leafy greens, turmeric, ginger, and omega-3-rich foods.
- Gut-healing Foods: Bone broth, fermented foods, and prebiotic-rich vegetables.
- Supplements
- L-glutamine: Repairs gut lining.
- Probiotics: Replenishes beneficial gut bacteria.
- Zinc Carnosine: Supports mucosal healing.
- Digestive Enzymes: Helps reduce gut strain during digestion.
- Lifestyle Changes
- Manage stress with yoga, meditation, or therapy.
- Prioritize sleep and exercise.
- Avoid smoking and excessive alcohol consumption.
- Medications (if necessary)
- Treat underlying infections or conditions (e.g., antibiotics for SIBO, medications for autoimmune diseases).
How to Test for Leaky Gut at Home
Can You Test for Leaky Gut at Home? While professional tests are more accurate, at-home testing kits are available and typically include:
- Urine sugar absorption tests (like lactulose/mannitol).
- Stool tests for gut microbiota analysis.
- Food sensitivity tests to identify triggers.
These tests can provide insight into gut health but may require follow-up with a healthcare provider.
Intestinal Permeability Diet
Eat more prebiotic foods, such as beans, onions, asparagus, oats, bananas, and other foods high in prebiotic fibers. Increase your probiotic intake to help your body produce more good gut bacteria. Yogurt, kimchi, kefir, and tempeh are all examples of foods that have undergone fermentation.
Otherwise, if you have leaky gut syndrome, you should avoid these foods: refined carbohydrates, glutinous grains, white sugar, dairy products, vegetable oils, artificial sweeteners, alcohol, and caffeine.
Bottom line
Although it might be challenging to distinguish the symptoms of increased intestinal permeability from the inflammation that comes before it, some people actually have this condition. When your gut lining is more permeable, bacteria living in your gut could cross the intestinal barrier, but we don’t know if this does significant harm separate from the original disease or injury that caused it. According to several research, liver disease may be caused by bacteria products that pass from the gut to the liver.
Intestinal Permeability (Leaky Gut) FAQs
1. What is intestinal permeability?
Intestinal permeability, often referred to as “leaky gut,” occurs when the intestinal lining becomes excessively porous. This allows undigested food particles, toxins, and bacteria to pass through the gut lining and enter the bloodstream, potentially triggering inflammation and other health issues.
2. What are the common symptoms of leaky gut?
Symptoms of intestinal permeability can vary but may include:
- Digestive issues (bloating, gas, diarrhea, or constipation)
- Food sensitivities or intolerances
- Fatigue
- Brain fog
- Joint pain
- Skin problems (e.g., eczema, acne, or rashes)
- Autoimmune conditions
- Mood disorders like anxiety or depression
3. How is leaky gut diagnosed?
There is no standard medical test for leaky gut, but several tests can help assess intestinal health:
- Zonulin levels: Zonulin is a protein linked to intestinal permeability. Elevated levels can indicate a leaky gut.
- Lactulose/mannitol test: Measures how these sugars pass through the gut lining.
- Stool tests: Can assess gut microbiota and inflammation markers.
- Food sensitivity tests: Identify foods that may aggravate gut issues.
4. What causes intestinal permeability?
Several factors may contribute to a leaky gut, including:
- Chronic stress
- Poor diet (high in processed foods, sugar, or alcohol)
- Overuse of NSAIDs or antibiotics
- Gut infections (e.g., candida, H. pylori)
- Dysbiosis (imbalance in gut bacteria)
- Autoimmune conditions
- Toxins, including pesticides and heavy metals
5. What dietary changes can help heal leaky gut?
A gut-healing diet often focuses on:
- Avoiding: Processed foods, refined sugars, gluten, alcohol, and food additives.
- Incorporating:
- Bone broth: Rich in collagen and amino acids for gut repair.
- Probiotic-rich foods: Yogurt, kefir, sauerkraut, kimchi.
- Prebiotic foods: Garlic, onions, bananas, asparagus.
- Anti-inflammatory foods: Fatty fish, turmeric, ginger, leafy greens.
- Gut-healing nutrients: L-glutamine, zinc, omega-3s, and vitamin D.
6. Are there supplements that support intestinal permeability repair?
Some commonly recommended supplements include:
- L-glutamine: Supports gut lining repair.
- Probiotics: Helps balance gut bacteria.
- Zinc carnosine: Enhances mucosal healing.
- Digestive enzymes: Aids digestion and reduces gut strain.
- Collagen peptides: Promotes gut lining repair.
- Omega-3 fatty acids: Reduces inflammation.
7. Can stress impact intestinal permeability?
Yes, chronic stress can disrupt the gut barrier, increase intestinal permeability, and alter gut microbiota. Stress management techniques like meditation, yoga, or therapy can help improve gut health.
8. How long does it take to heal a leaky gut?
Healing can take anywhere from weeks to months, depending on the severity and underlying causes. Consistency in dietary, lifestyle, and supplement interventions is key.
9. Can leaky gut lead to other health problems?
Leaky gut is associated with various conditions, including:
- Autoimmune diseases (e.g., Hashimoto’s, rheumatoid arthritis)
- Irritable bowel syndrome (IBS)
- Food intolerances
- Allergies
- Skin disorders (e.g., psoriasis, eczema)
- Chronic fatigue syndrome
10. When should I consult a doctor about leaky gut?
If you have persistent symptoms like digestive distress, unexplained fatigue, or chronic inflammation, consult a healthcare provider. They can evaluate your symptoms, test for underlying conditions, and recommend a tailored treatment plan.
Share:


